Abstract
Background: Currently, systemic steroid therapy remains the first-line treatment for the management of Chronic Graft Versus Host Disease (cGVHD); however, in refractory patients, the second-line option is not standardized and remains challenging. In this study, our objective was to compare the overall survival (OS) between the different options available for the secondary systemic treatment of patients who develop cGVHD in the northeast of a country with limited resources.
Methods and Objective: Patients >16 years old who underwent allogeneic HSCT from 2015 to 2021 in our center with any hematological disease were included. Conditioning was based on cyclophosphamide, fludarabine, and melphalan or busulfan, and we used peripheral blood in all cases. Clinical files and electronic databases were analyzed to document the number of patients who developed cGVHD according to the histopathological diagnostic criteria described in the National Institutes of Health (NIH) Consensus Conference, as well as the time after transplantation in which systemic treatment was started, the different lines of treatment used, the grade, weekly clinical stage of cGVHD and the immunosuppressive treatment used.
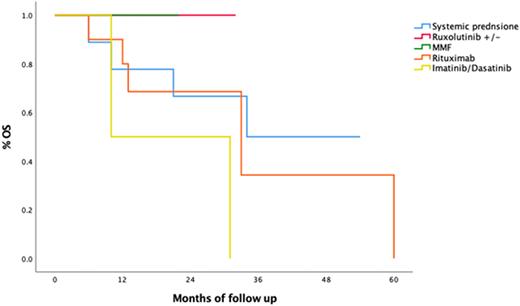
Results: We analyzed 199 consecutive transplants; 75 (37.68%) developed cGVHD, and the median number of days for the start of systems related to cGVHD was 148 days (23-707). More than half of the patients did not respond to first-line treatment with systemic glucocorticoids (n=36,61.7%). Of non-responders, second-line therapy was started at a median of 22 days after initial treatment. The different second-line treatments reached five different schemes, as shown in graph 1. Twenty-five (34%) patients with cGVHD received 3 or more lines of therapy. Ten months after the start of second-line therapy, 10 patients (42%) were alive. The best treatment regimen that demonstrated to improve survival was low-dose Rituximab (100 mg every week for 4 weeks) with an OS of 80% at twelve months of follow-up (p=0.03). Overall mortality was 40.7% (81 patients), relapse-related mortality was 50.6% (41 patients), and non-relapse mortality (NRM) was 49.4% (40 patients). Of the latter, 43% (15 patients) were due to infection, 20% (7 patients) were associated with cGVHD, and 37% (13 patients) were due to other causes.
Conclusions: We identified a slightly higher incidence of cGVHD than that reported in the international literature, probably because of the use of peripheral blood as a source of stem cells and a higher frequency of haploidentical transplants. It was also evidenced that systemic steroid therapy is not sufficient for a considerable proportion of patients who will be refractory; for them, the best results were achieved with the scheme based on low-dose Rituximab, which improved the final results even with an advantage over those patients who received tyrosine inhibitor therapy (ruxolitinib/dasatinib/imatinib). Despite this, it is necessary to continue exploring feasible and accessible therapeutic options for our type of population with prospective controlled studies that reduce NRM secondary to the graft and the infections associated with its immunosuppression.
Disclosures
Gomez-De Leon:AbbVie: Honoraria, Other: advisory board. Gomez-Almaguer:Takeda: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; BMS: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal